When Justin Timberlake revealed that he’s been battling Lyme disease on Instagram, it lit up the internet. Some people sent well-wishes, others asked questions about the illness, and a few—of course—propagated bucket loads of misinformation. Given the internet’s natural inclination to run with rumors and unchecked theories and the considerable amount of confusion online over what Lyme disease is, how it gets diagnosed, and what causes it. There are also some absolutely bonkers conspiracy theories, but we’ll get to that later.
According to the U.S. Centers for Disease Control and Prevention (CDC), Lyme disease, in the most basic sense, is a bacterial infection spread through the bite of blacklegged ticks, most common in the United States. “A tick bites you and burrows into [your skin],” Donald Dumford, an infectious disease specialist for the Cleveland Clinic, tells The Daily Beast. “After it’s been attached for a couple of days, the tick ends up transmitting the bacteria.”
Timberlake, who has been in the entertainment industry for three decades since the 1995 formation of N*SYNC, wrote on Instagram that performing in his two-year “The Forget Tomorrow World Tour” while battling the disease was “at times, [a] grueling experience.” Writing to his 72.1 million followers, the 44-year-old singer described Lyme disease as “relentlessly debilitating, both mentally and physically.” Still, the diagnosis offered long-awaited clarity, finally explaining the nerve pain, “crazy fatigue,” and persistent illness he had been struggling with.
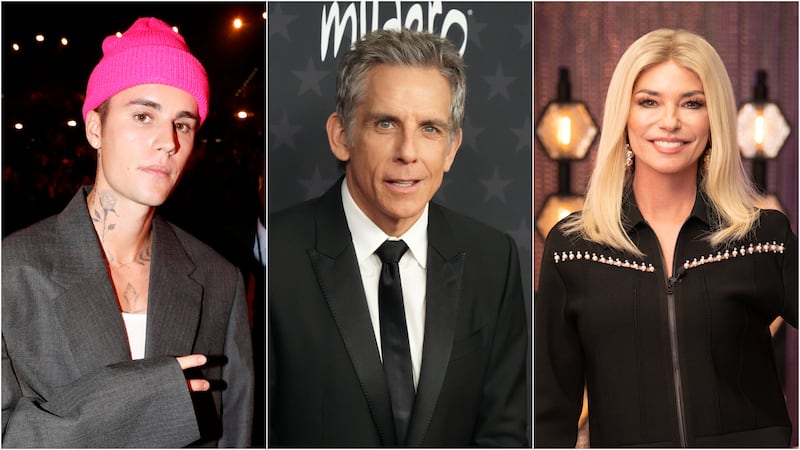
The ex-boy bander is not the only celebrity to reveal a diagnosis: Justin Bieber, Shania Twain, and Ben Stiller have all shared their journeys battling the disease publicly.
Timberlake’s winding path to a diagnosis is far from unique, and it’s drawn attention to an often misunderstood condition. Many people living with Lyme disease don’t even know they have it, as the condition is frequently misdiagnosed or overlooked entirely. To get to the truth and cut through the confusion—and to learn the best ways to avoid Lyme disease as much as possible—I consulted with infectious disease specialists and emergency physicians.
What is Lyme disease, and how do you get it?
The illness is caused by a “spirochete type of bacterium that gets into your body,” explains Mark Conroy, an emergency medicine physician at the Ohio State University Wexner Medical Center, most notably through infected black-legged deer ticks in the northeast, mid-Atlantic, and north central regions of the U.S.
A tick bite doesn’t mean instant infection, however. According to Edward Liu, an infectious disease specialist and the section chief of infectious diseases at Hackensack Meridian Jersey Shore University Medical Center, it typically takes about 36 hours for a tick to transmit Lyme disease after latching on.
In the majority of cases, around 70 to 80%, patients with Lyme disease report a bull’s-eye rash as the first tell-tale sign post-bite. Dr. Dumford says this usually occurs within the first week before “secondary issues” arise two to four weeks into the infection. If still undiagnosed, some people develop more persistent types of infections that can be “intermittent and have varying degrees of joint inflammation,” and sometimes chronic, says Dr. Dumford.
According to Dr. Liu, milder symptoms include some fever, fatigue, and achiness, similar to the flu. “[Lyme disease] mimics a lot of different things,” Dr. Liu says, which can often delay proper diagnosis if not caught in the early stages.
More serious problems can occur as the infection spreads throughout the body, affecting the joints, nervous system, and heart. When the infection spreads unchecked, complications like septic arthritis, carditis, and heart block can develop, underscoring the importance of early detection. In some instances, the disease can even prompt meningitis-like symptoms, involving inflammation of the membranes and fluid surrounding the brain and spinal cord.
How doctors detect and diagnose Lyme disease
“We start with an initial antibody screen,” Dr. Dumford explains, “then we have to confirm it through a western blot,” which is essentially a laboratory technique used to detect the weight of proteins a patient has. A Western blot is used during diagnosis to confirm an initial positive test by checking for the specific pattern of proteins, helping to rule out a false positive.
“When you have that initial test, or a screening test, you’re trying to catch as many positive tests as possible,” says Dr. Dumford. If the parameters of the initial test are too narrow, doctors may “miss some truly positive ones,” which is why these tests can be “overly sensitive,” and why a secondary test is necessary.
While testing is considered reliable, diagnosing diseases caused by infections can present unique challenges. “The concern is that, since we’re dealing with an antibody test, you need about four weeks, or even up to six weeks, for the body to start to make antibodies,” says Dr. Dumford. “I always teach my students and residents: If somebody has Lyme disease—let’s say they get that classic rash early on, or they’re having those secondary manifestations—you treat them and check for antibodies [at that time] and again in four weeks.”

“So, if you test someone early in the course, it might come back negative—even though they do have Lyme disease,” Dr. Conroy says.
Dr. Liu emphasizes the importance of physicians and providers “asking the right questions” to confirm diagnoses, as well. The symptoms of Lyme disease vary widely, so it’s not uncommon for patients to initially receive incorrect diagnoses, such as fibromyalgia, osteoarthritis, or meningitis, depending on how Lyme disease manifests in a patient.
How Lyme disease is treated
When you get treated properly, the current understanding amongst the medical community is that the bacterium is gone. Similar to observations of long-COVID symptoms, even after the infectious disease has been treated, some patients have documented long-term symptoms, including fatigue, dizziness, and chronic joint pains.
The primary course of action in treating this disease is antibiotic prescriptions, which must then be taken for a regular duration. A medicine called doxycycline is “the cornerstone of therapy,” says Dr. Dumford. This is because it is highly effective for this bacterium as well as the co-infection caused by the tick. Other antibiotics, such as amoxicillin, can be prescribed as an alternative treatment for someone who can’t take doxycycline (for instance, those who are allergic to it).
For brand new infections, Dr. Liu asserts that two weeks of regular antibiotics should do. In contrast, in more serious cases where regions such as the heart are impacted, three to four weeks of antibiotic treatment is recommended. “Most infections doctors won’t treat you longer,” he says.
There are always exceptions to the rules, of course, in severe cases of Lyme meningitis, doctors “stick with intravenous antibiotics,” says Dr. Liu, because of their increased ability to target the brain better. It’s important to note that Lyme disease can be eliminated with these courses of action. “There’s no evidence of consideration that [Lyme disease] becomes dormant,” Dr. Conroy tells The Daily Beast.

What is post-treatment Lyme disease syndrome, and is it different from “chronic Lyme disease”?
This “Chronic Lyme disease” refers to a constellation of symptoms that are harder to attribute to Lyme disease because they mimic other conditions. These symptoms often include fatigue, fever, and muscle weakness. Patients may not have any of the bacterium still in their body or joint fluids, but still experience the symptoms. “I would never disagree with what someone is feeling,” Dr. Conroy says. “But it’s not because the bacteria are actively in their body causing problems.”
According to the CDC, “It is especially unlikely that Lyme disease is the cause of prolonged or recurring symptoms if you tested negative … using a recommended test or have not lived in or traveled to areas where Lyme disease is common.”
According to a paper published in Clinical Reviews of Allergy & Immunology authored by Katelyn H. Wong, Eugene D. Shapiro, and Gary K. Soffer, the term “chronic Lyme disease” is a poorly defined phrase that is “used to describe patients with nonspecific symptoms…attributed to the presumed persistent Borrelia burgdorferi infection in patients who may or may not have evidence of either previous or current Lyme disease.”
The term “post-treatment Lyme disease syndrome” is an accurate descriptor—and one that is used by physicians—for describing the condition, as it refers to patients who continue to experience long-term symptoms after receiving proper treatment for Lyme disease. “You’ve got to say, ‘Okay, we’ve diagnosed Lyme disease, we’ve treated it,’” Dr. Dumford explains. “And if there are still those persistent symptoms, we can say the patient has [post-Lyme syndrome].”
The CDC notes that if someone has already had their Lyme disease treated using antibiotics and continues to struggle with the symptoms mentioned above, “studies have shown that more antibiotics are unlikely to help.”
What to do if you find a tick on you
Despite your best efforts, it’s happened: you discovered a free-loading tick has made its way onto your skin. First, take a deep breath. Then, take action.
Identification and removal are important, so take care when doing both. “If you pull a tick off, get tweezers and make sure you get really close to the skin,“ says Dr. Dumford. ”You want to make sure you pull the head out, as well, because you can still have mouth parts [there] that might actually cause irritation.“ He suggests either sending the tick to a lab for identification or consulting a reliable online source, such as the website for the CDC or your state’s health department, which will often have pictures of different types of ticks.
Prevention tips for avoiding Lyme disease
Whether you’re an avid camper, a fan of hiking, or just enjoy the outdoors once in a while, taking steps to prevent contracting Lyme disease is incredibly important.
Wooded areas, low-growing grasslands, and everyday yards are where these ticks prefer to inhabit. While a year-round issue, April to October are generally the months to be on high alert regarding tick season and warmer temperatures, where people are more likely to venture outside.

Citizens in northeast states like New York, New Jersey, Rhode Island, and Massachusetts, and especially Connecticut (Dr. Conroy referred to it as a historical center for the disease), should be wary. Though with climate change, increased travel, and other external factors, more cases are moving westward in states like California and Pennsylvania.
Dr. Conroy recommends being smart about where you’re hiking, wearing long pants in the woods, using appropriate bug sprays, purchasing ointments that prevent ticks from biting, and checking your body for bites after spending time outside. Tucking long pants into socks can help spot a tick before it attaches. Wearing EPA-approved insect repellents—like DEET-based sprays or eucalyptus oil—and treating clothing with permethrin, a synthetic insecticide that disrupts tick movement, are also effective preventative measures, according to Dr. Dumford.
The evolving understanding of Lyme disease underscores the importance of accurate diagnosis and adherence to recommended treatment protocols. As medical professionals strive to improve patient outcomes, awareness and prevention remain key components in addressing this persistent public health concern.
Wait, what were those “conspiracy theories” you mentioned?
While we’re almost reluctant to share these (and, truthfully, are choosing to exclude many of the wildest theories), we trust that, after reading all of the above expert-provided information, you’ll recognize their absurdity. To be clear, these theories are unproven and unscientific. Always refer to reputable sources and medical experts for information.
A few “milder” pieces of misinformation—albeit still dangerous—include untested and unproven theories such as Lyme disease can be transmitted sexually and that Lyme disease causes Autism, Alzheimer’s disease, multiple sclerosis, and a plethora of other diagnoses. For obvious reasons, we aren’t linking out to sites that promote pseudoscientific theories, but researchers have published peer-reviewed papers that critically examine some of these claims and offer a plethora of science-backed data and reporting to counter them.
There are also people who believe Lyme disease is an “escaped military bioweapon,” according to a 2019 article in The Conversation written by Sam Telford, an infectious disease and global health professor at Tufts University, who used his expertise to debunk the rumor soundly.
The truth about Lyme disease
Lyme disease is real, and it’s crucial that you take preventative measures when spending time outside. If you catch a tick in the act, or suspect you’ve been bitten, get checked out. Oh, and don’t believe everything you hear on the internet.
The post The Truth About Lyme Disease, the Illness Justin Timberlake Was Diagnosed With appeared first on The Daily Beast.




