There goes the neighborhood!
Suburban living has its upsides — bigger homes, less noise and more natural green spaces, to name a few. Developments with grassy lawns and wooded parks draw families because they create a sense of relaxation and offer safe areas for children to explore and play, boosting physical and mental health.
But some creepy, clingy intruders pose a threat to these serene settings by transmitting disease and even sparking an unusual allergy to red meat.

Certain ticks can trigger alpha-gal syndrome (AGS), a possibly life-threatening allergic reaction to beef, pork, lamb or other animal products.
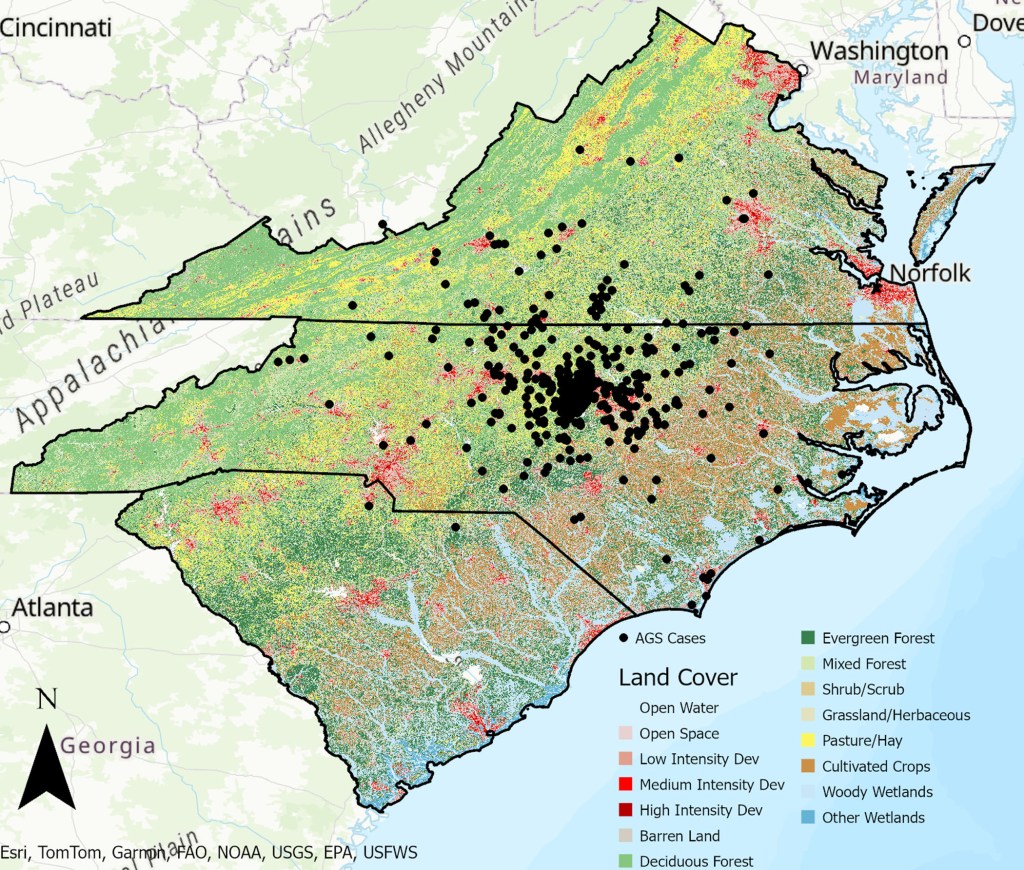
Scientists from the University of North Carolina at Chapel Hill say they have identified potential environmental drivers of AGS risk by mapping 462 confirmed cases in North Carolina, South Carolina and Virginia.
“Since the first documented case in the southeastern US in 2009, diagnoses of AGS have increased rapidly, with reported cases increasing from 24 in 2009 to over 34,000 in 2019,” the researchers wrote last week in the journal PLOS Climate.
“AGS is the leading cause of adult-onset allergies in the US, with test positivity rates of 30.5%.”
Tick saliva contains alpha-gal, a sugar molecule found in red meat. A tick bite introduces alpha-gal into the bloodstream, tricking the immune system into thinking red meat is harmful.
Symptoms, which typically emerge two to six hours after eating meat, include hives, nausea, wheezing, low blood pressure and fatigue. Severe cases may lead to anaphylaxis, requiring immediate medical attention.

The lone star tick is the most common culprit for AGS, though deer ticks also have been implicated.
Lone star ticks are primarily found in the southeastern, south-central and mid-Atlantic regions of the US — they are especially abundant on Long Island, particularly Suffolk County.
UNC computer models showed that open space development, defined by large swaths of natural areas, and forests with a mix of trees pose the greatest AGS risk.
Ticks thrive in warm, moist environments. They like to hide in tall grass and shrubs to ambush passing animals like deer, rodents and birds.
“Understanding environmental factors affecting AGS risk is important for identifying at-risk populations for intervention strategies (e.g., educational campaigns and diagnostic testing),” the UNC study authors said.
It’s unclear how many new AGS cases have been logged this year.
The researchers noted that AGS often goes underreported because the Centers for Disease Control and Prevention does not require healthcare providers to report suspected cases.
How to prevent tick bites
Tick season in New York typically runs from March to November, with peak activity from April to September.
NYC Health + Hospitals has several recommendations for reducing the odds of contracting a tick-borne illness like AGS, Lyme disease or babesiosis.
- Cover as much skin as you can by wearing a hat, long sleeves and gloves and tucking shirts into pants and pants into socks.
- Wear light-colored clothing, so it’s easier to notice ticks on you.
- Apply insect repellent to clothes, exposed skin and outdoor gear.
- Check yourself, children and pets for ticks before coming inside.
- Wash clothes in hot water and tumble them in a dryer on high heat to kill ticks.
- Shower within two hours.
- If you spot a tick, carefully remove it with tweezers, put it in a sandwich bag and place it in the freezer in case it’s needed for identification.
- Wash the bite area with alcohol or soap and water.
- Watch for symptoms such as fatigue and numbness in the arms and legs, fever, chills, rash, headache or joint pain.
The post How living in the suburbs can increase your risk of developing a meat allergy appeared first on New York Post.




