Gen Z-Backed Rapper Is on Course to Lead Nepal With Landslide Win
In a resounding affirmation of Gen Z’s power to overthrow the political old guard, Nepali voters have handed a commanding...
Trump Steamrolls Pentagon Pete With Wild War Claim
In a rare show of disagreement, Pete Hegseth failed to echo boss Donald Trump’s claim about the ongoing conflict in...
These robots are coming for the jobs no one wants — and could fill workforce gaps
Agility Robotics' Digit operates inside a GXO facility. Courtesy Agility RoboticsAgility Robotics is deploying humanoid robots at Toyota's Canada manufacturing...
‘SNL’ leaned into Ryan Gosling’s giggles in his fourth stint as host
They knew he was going to break. And they leaned into it. That’s the only explanation for this week’s Ryan...
I’ll Buy That: The Joy of Having Fun With Fashion
The big stuffed fish perched suggestively on one of the white seating cubes with its fins crossed probably should have...
This AI founder who quit her 9-to-5 law job has a warning for anyone dreaming of doing the same: ‘I’m working harder now than I ever did’
Office workers who daydream of being their own boss may fantasize about calling the shots, earning sky-high salaries, and setting...
Scientists Taught a Clump of Human Brain Cells to Play Doom
The internet has a long, rich history of getting the classic video game Doom to play on a wide variety...
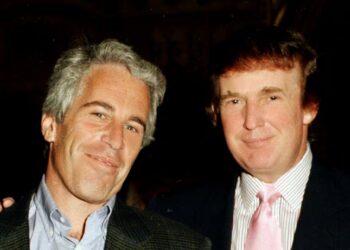
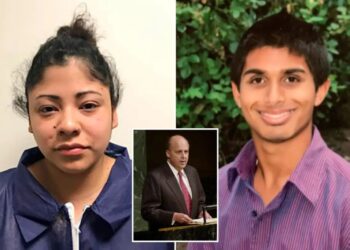
FBI Met Four Times With Woman Who Said Trump Assaulted Her When She Was 13
A woman who accused Donald Trump of sexually abusing her when she was 13 was interviewed by FBI agents four...
My strange, sleep-deprived week hobnobbing with the global elite
Jason Sanchez/BIIt started with a mysterious slack from our editor-in-chief, Jamie Heller: Can you talk now? It was the kind...
Etiquette expert reveals 5 common coffee shop habits that customers need to stop
Coffee shops may feel cozy and casual, but one etiquette expert says too many customers forget they are still shared public spaces....