Your risk of developing dementia may be more closely tied to your ZIP code than you think, according to a large-scale study of U.S. military veterans aged 65 and older.
Analyzing health data from over 1.2 million veterans who received care through the Veterans Health Administration (VHA) between 1999 and 2021, researchers found that where someone lives can significantly influence their chances of developing dementia—even after accounting for age, race, heart disease, diabetes, and whether they lived in rural or urban areas.
The study revealed stark regional differences. Veterans living in the Southeast faced the highest risk, with dementia rates 25 percent higher than those living in the Mid-Atlantic, the region with the lowest rates.
Other high-risk areas included the Northwest and Rocky Mountains, where dementia risk was 23 percent higher than in the Mid-Atlantic. The South, Southwest and South Atlantic also showed elevated rates.
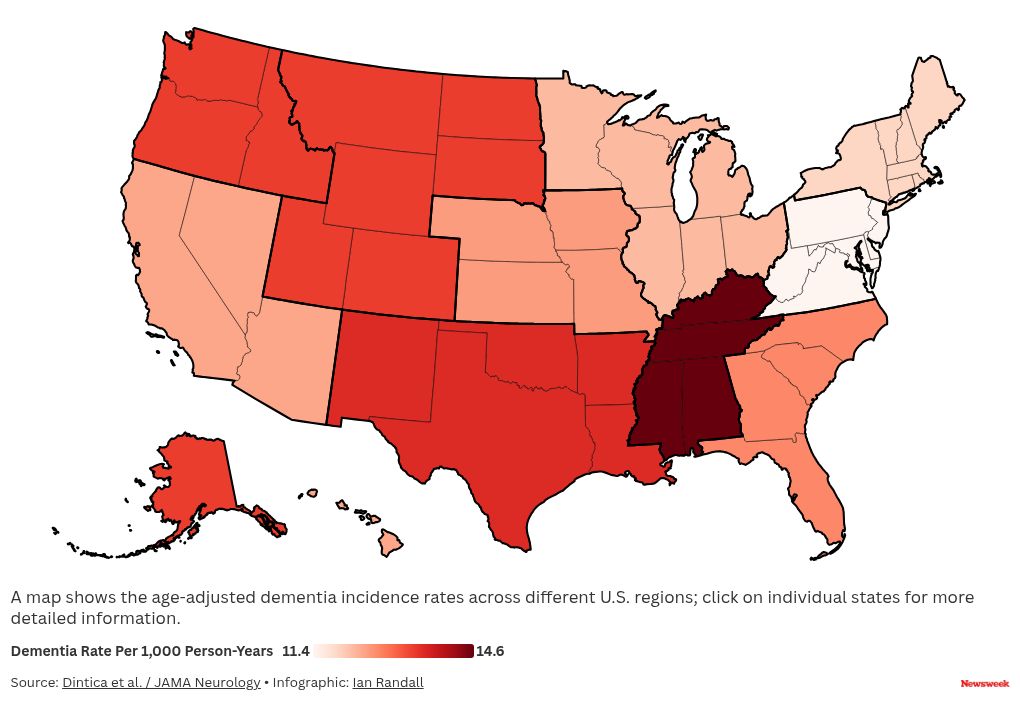
The researchers measured how many new cases of dementia were diagnosed each year per 1,000 people. In the Southeast, that number was 14 cases per 1,000 person-years, while in the Mid-Atlantic it dropped to just 11.2. Even after adjusting for factors like demographics, rurality and cardiovascular conditions, the regional patterns remained consistent.
“The study underscores the need to understand regional differences in dementia and the importance of region-specific prevention and intervention efforts,” said senior author Dr. Kristine Yaffe, also of the San Francisco VA Health Care System, in a statement.
What Might Be Driving the Regional Differences?
Researchers explored why dementia rates varied so widely across regions, and several key factors may help explain the gap.
Although health, age, and environment clearly play a role, the data showed that geographic location remained a strong predictor even after accounting for those variables, suggesting there’s more going on beneath the surface.
Potential Factors Influencing Dementia Risk:
- Education: Lower educational attainment was more common in regions with higher dementia rates.
- Health Conditions: Chronic illnesses such as stroke, high blood pressure, diabetes and obesity were more prevalent in higher-risk areas like the Southeast.
- Lifestyle and Environment: Smoking and other regional lifestyle patterns may contribute.
- Access and Quality of Health Care: While the VHA generally offers more equal care across regions, differences in resources and specialty care at individual VA centers may affect how—and whether—dementia is diagnosed.
- Diagnosis Practices: Studies using Medicare data suggest that how often and how well dementia is diagnosed can vary, not just because of patient health but also due to how local health systems operate.
- Hidden Variables: Some important influences—such as quality of early-life education or early signs of cognitive decline not captured in health records—may not show up in administrative data but could still drive long-term risk.
All-in-all, the study makes one thing clear: location matters. While individual lifestyle choices and genetics remain important, where you live could shape your brain health more than previously understood.
These findings underscore the need for more localized research and targeted interventions, especially in regions facing higher dementia burdens.
Understanding why dementia hits harder in some areas than others is essential—not only for treating the disease but also for preventing it in the first place.
Do you have a tip on a health story that Newsweek should be covering? Do you have a question about dementia? Let us know via [email protected].
Reference
Dintica, C. S., Bahorik, A. L., Xia, F., Boscardin, J., & Yaffe, K. (2025). Regional differences in dementia incidence among US veterans. JAMA Neurology. https://doi.org/10.1001/jamaneurol.2025.1536
The post Map Shows States Where Dementia Risk Is Highest appeared first on Newsweek.




