Blood sugar is a hot topic, and after months of watching content waxing lyrical about “balancing it,” I needed to know if it was true that tracking my glucose levels would help boost my energy.
So with a few taps on my laptop, I ordered a continuous glucose monitor: a small white disk carrying a tiny needle, which charts blood sugar levels in near real-time via an app.
Designed for people with diabetes to closely monitor their glucose levels and prevent potentially life-threatening fluctuations, in recent years, they’ve become a buzzy lifestyle wearable marketed at healthy people.
Glucose is our primary energy source, which we get from carbohydrates in food and drink. The body uses it for energy, and anything that’s left over is stored in the muscles, liver, or fat cells for later use. Sugary snacks and simple carbs like white pasta tend to lead to bigger blood sugar spikes, while pairing carbs with protein, fats, and fiber has been found to smooth out the curve.
The term “glucose spike” has become a dirty word, as wellness influencers say that peaks and troughs lead to weight gain, energy crashes, and cravings. In turn, there are plenty of personal anecdotes online — but limited evidence — that “balancing” blood sugar by keeping it stable has helped people lose weight, feel happier and more energetic, sleep better, and avoid chronic disease.
Despite following a pretty balanced diet — I eat protein and plenty of fiber with most meals, and few ultra-processed foods — I’m often tired and lacking energy. I was curious to see if the longevity bros were onto something, and if wearing a CGM for two weeks could provide any helpful insights.
By the end of the experiment, I felt like I was in sugar jail.

Tracking my blood glucose levels was exciting at first
The experience started with the sharp scratch of the CGM needle puncturing my skin. I held the plastic applicator to the back of my left arm, pressed down, and before I knew it, was branded with a white plastic circle. It stayed there for two weeks, measuring the glucose levels in the fluid around my cells and sending the data via Bluetooth to a line chart on my phone. I felt very aware of the CGM when my arms were exposed in public, which made me feel a little self-conscious.
At the beginning, it was exciting having access to this new metric, and the first thing I did was eat a rich chocolate truffle.
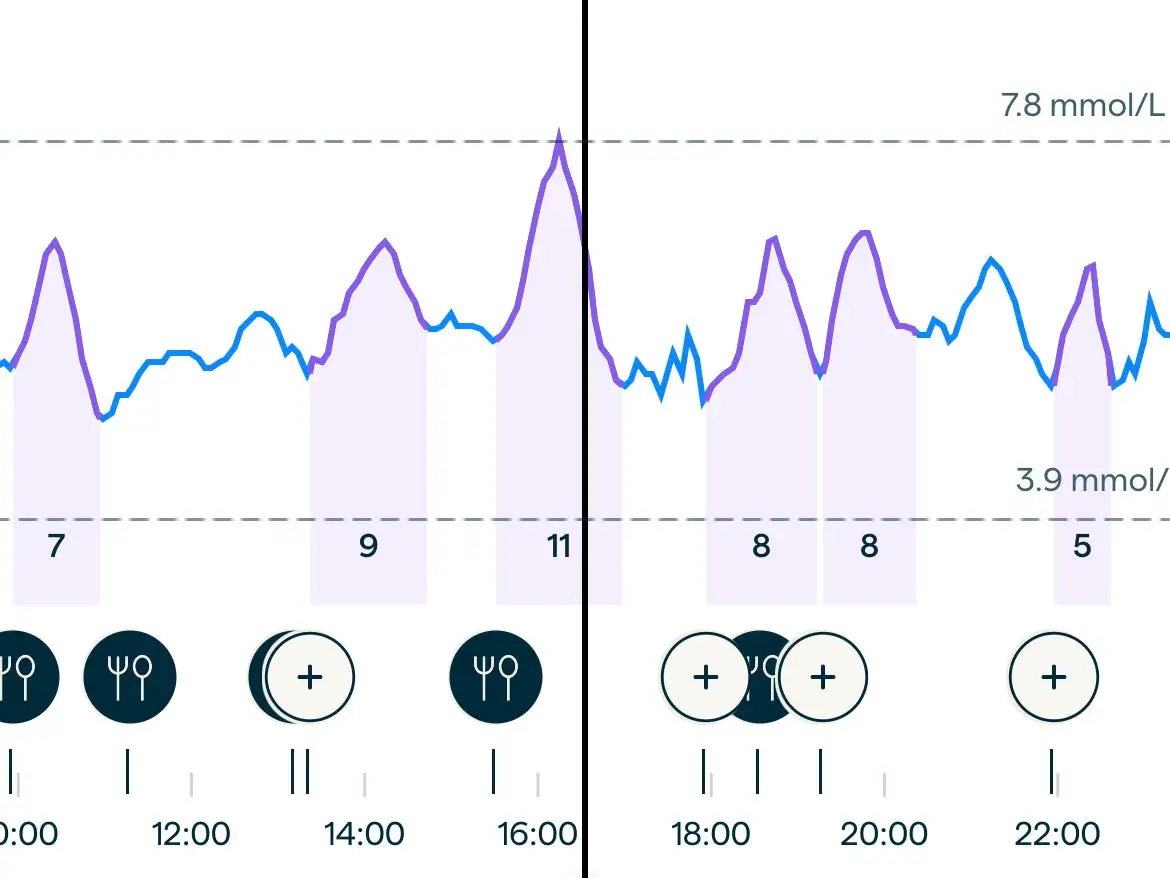
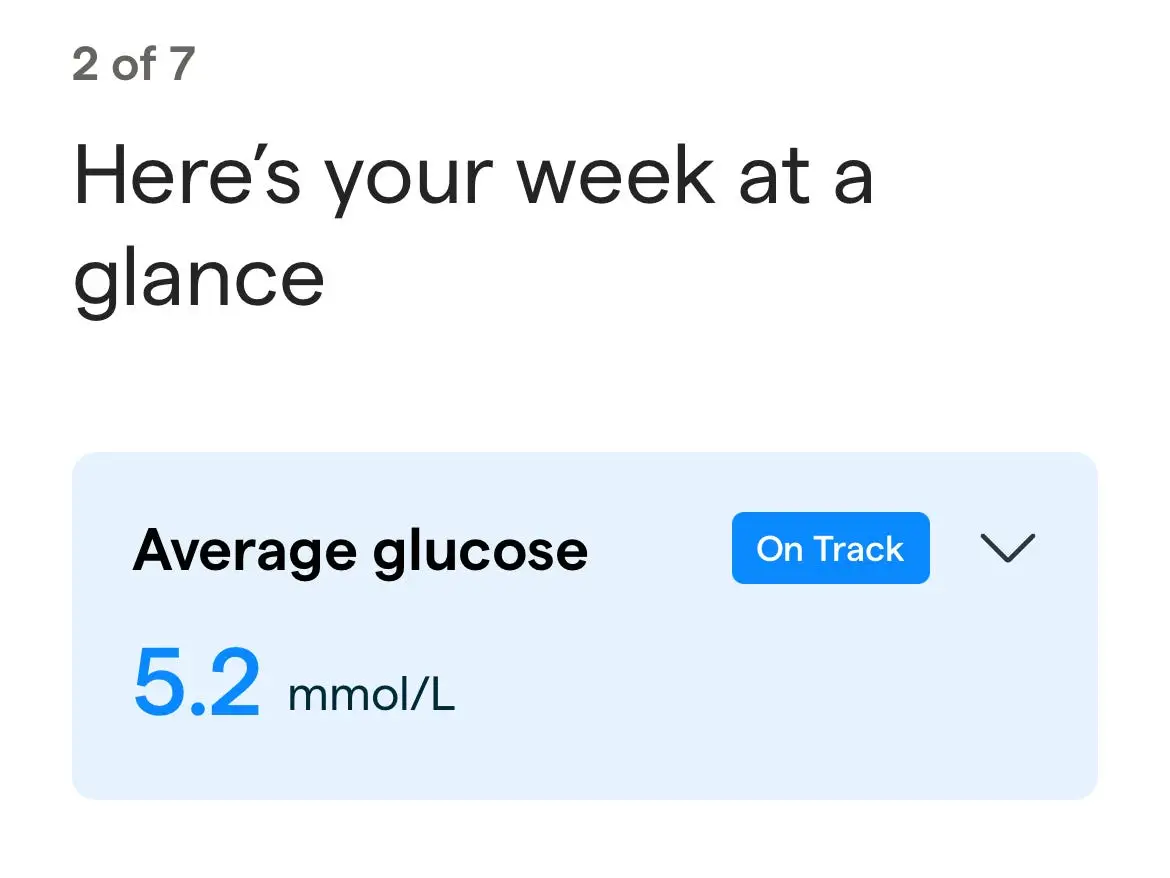
Unsurprisingly, the little line on the chart — representing my glucose level — started moving sharply up, but I was pleased to see that it stayed within the healthy range of 3.9 mmol/L to 7.8 mmol/L. This was delineated on the chart by two dotted lines, which made it easy to see if I was having what would be considered a glucose spike or dip.
The line moved every time I ate or drank something other than water, exercised, or felt stressed (both can affect glucose levels).
I started interpreting my glucose levels as ‘good’ or ‘bad’
I ate normally to get an idea of my typical daily blood glucose levels, and in hindsight see that I quickly fell into the trap of judging meals as “good” or “bad” based on their effect. I know that’s not a healthy way to think of food, but I guess I subconsciously believed the reductionist idea that any rise in blood sugar should be avoided. In fact, fluctuations within the healthy range (and sometimes outside of it) are just a normal part of digestion.
So I was pleased when my go-to breakfast didn’t cause a spike, but surprised when the flat white coffee with 2% milk that I drank before it caused the level to rise as much as my entire breakfast.

I didn’t love that my protein and fiber-rich lunch of ground turkey and black bean chili with red rice sent my line close to the top of the healthy range, but reasoned that was probably because it was larger than my breakfast. I felt particularly disheartened when a dinner of soba noodles, which are made from buckwheat flour (complex carbs), and tofu (protein) in broth with cabbage (fiber) marked the first sharp spike.
I was even more confused when the chili caused a huge spike and the noodles didn’t when I ate the same lunch and dinner the next day.
My blood sugar didn’t exceed the healthy range many times, but when it did, it was after I consumed:
- a mocha with whole milk on an empty stomach
- a packet of lentil chips
- chicken nuggets
- a mushroom Wellington with roast potatoes, cauliflower cheese, and cavolo nero
- baked salmon marinated in mirin with Japanese rice, green beans, and broccoli
- tuna whole wheat pasta bake

I would consider half of these balanced meals, but according to my chart, they raised my blood sugar more than the sweet treats like cake and a brownie that I ate during the two weeks. Maybe that’s to be expected, but, without an expert to explain the data, I didn’t know.
On reflection, I underestimated how complicated it would be to decipher this data and apply it to my life healthily. My glucose levels fluctuated more than I expected and it wasn’t always clear to me why.
The app did explain that a healthy person’s blood sugar tends to be outside of the healthy range for up to two hours per day, but I wasn’t sure if an unsteady line within the safe zone was worrying or not (a nutrition researcher I spoke to since reassured me that it is not).
In terms of my energy levels, I noticed that I felt better on weekdays when I ate three square meals a day around the same time than weekends, when I tended to skip breakfast and eat a big meal around 2 or 3 p.m. This was reflected in my blood sugar levels, but I’m not sure I needed a CGM to figure that out.
When my blood sugar rose, the app would tell me to do calf raises for 5 to 10 minutes
The urge to check how my body reacted to food after a few bites quickly became a compulsion. Even though I understood a spike wasn’t necessarily bad, I still felt encouraged by the app to keep my line as straight as possible.
It set me a daily target to stay within, at first based on averages and after a week based on my levels. It would tell me to do 15 squats, five to 10 minutes of calf raises, or take a brisk walk, when my glucose started rising (research suggests these movements can bring it down). I tried to go on walks, and did the squats on two occasions, but I drew the line at 10 minutes of calf raises.
The app was purportedly helping me to make my diet even healthier, but I became hyperfixated on a single metric that I didn’t really understand.
I felt a pang of dread every time I ate, knowing my glucose levels would rise and the app would watch and prescribe me exercise like some kind of punishment. It felt like the only way to keep my glucose stable would be to unnecessarily overhaul my already healthy diet.
Health optimization feels like a trap
I intended to spend the second half of the experiment trying to avoid spikes and observing if I felt more alert and focused. That was before I realized that optimizing your health means aiming for constantly shifting goal posts. Once you perfect one metric, you simply move onto the next.
Having too many blood sugar spikes over time can increase the risk of obesity, type 2 diabetes, and heart disease. But diabetes experts previously told Business Insider that glucose monitoring isn’t necessary for people without the disease and that it can cause unnecessary anxiety.
It’s possible that cutting out all refined sugar and eating plainer, simpler meals would help me focus a little better. But I already track my sleep, go for a daily lunchtime walk, do a weekly run, eat 30 plants a week, and stop drinking caffeine after 1 p.m, in the name of my health.
Maybe it was the invasive nature of sleeping with a needle in my arm, or the Black Mirror-ness of my phone tracking my bloodwork, but I suddenly felt I was on the border between healthy and obsessive. That isn’t somewhere I want to be.
Read the original article on Business Insider
The post I tracked my blood glucose levels for two weeks. It felt like I was in sugar jail. appeared first on Business Insider.