You’re reading The Checkup With Dr. Wen, a newsletter on how to navigate medical and public health challenges. Click here to get the full newsletter in your inbox, including answers to reader questions and a summary of new scientific research.
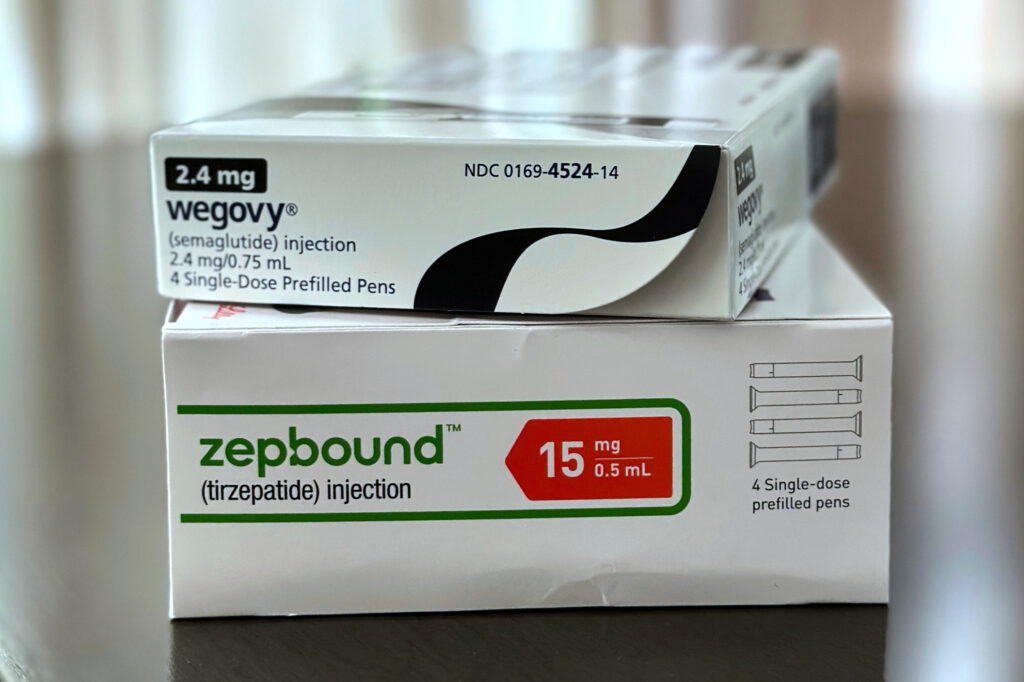
Last week, I focused my column and newsletter on GLP-1s, the highly effective medications used to treat obesity, Type 2 diabetes and a growing list of related complications. Many readers shared their personal experiences with the drugs, while others had additional questions. I’m dedicating this newsletter to highlight those stories and address their queries.
Marc from Louisiana, a 70-year-old practicing physician, is among many who recounted the enormous difference GLP-1s have made in their lives. “I was also very active in competitive tennis leagues and tournaments up until covid hospitalized me in late 2020.” he wrote. “I gained about 40 pounds (up to 243 pounds) since then. I felt like I couldn’t diet and exercise my way out of this weight gain and bit the bullet and started taking tirzepatide. I’m 26 weeks in. I’ve lost the 40 pounds, and I feel much better. I’m able to cycle and lift weights, and I hope to regain some of the fitness that I’ve lost. … I’m also down to only one anti-hypertension medication.”
Margaret from Calgary, Alberta, shared that she had been overweight most of her life. By her 50s and 60s, she was 5 feet tall and weighed 324 pounds, despite trying many diets and medications. With GLP-1s, however, she reduced her weight to about 138 pounds. “Semaglutide has been a lifesaver for me,” she wrote. “My bloodwork has never been better, my cholesterol is now normal, my liver enzymes are normal, I no longer have fatty liver disease, my arthritis is much more manageable, as is my asthma. In fact, every facet of my life has improved despite being diagnosed with breast cancer and Parkinson’s. I shudder to think what my life would be like now in my mid-70s without these miracle medications.”
Ana from Indiana wrote that she and her husband had been trying to conceive for more than 10 years. “We tried and failed several rounds of in vitro fertilization, then gave up because it was too heartbreaking. Two years ago, my doctor recommended that I start semaglutide for weight loss and prediabetes. Lo and behold, I got pregnant and am now the mom of a beautiful baby girl! I found a lot of stories on the internet for women with this experience. Is this just anecdote or is there an actual reason behind it?”
Congratulations, Ana! Indeed, many women have reported becoming pregnant after starting GLP-1s, and scientists have a theory for why that’s the case: Excess weight can disrupt hormones that control ovulation, leading to irregular or absent menstrual cycles. For instance, one common cause of infertility is polycystic ovary syndrome, a condition marked by hormonal irregularities and insulin resistance.
By improving insulin sensitivity and promoting weight loss, GLP-1s can help regulate ovulation. Early research has found that women with PCOS who take these drugs may see improvements in hormonal balance. Larger studies are now underway to confirm whether GLP-1s might be a treatment for infertility linked to metabolic and hormonal factors.
Misty in New Hampshire said that her physician recommended both menopause hormone therapy and a GLP-1 to manage menopause-related weight gain. “Is this a good idea — is it safe to combine these treatments?”
Yes. In fact, research suggests the two therapies complement one another. During the menopausal transition, declining estrogen levels change how the body stores and burns fat, often leading to increased abdominal weight. Hormone therapy helps restore some of estrogen’s metabolic effects, improving fat distribution and preserving lean mass, while GLP-1s work through a different pathway, by reducing appetite, slowing digestion and improving blood sugar control.
A study published in the journal Menopause last year found that postmenopausal women taking semaglutide while on hormone therapy lost significantly more total body weight over 12 months than those not on hormone therapy. Another study reported comparable results for tirzepatide. For women who are appropriate candidates for both, the combination appears safe and might enhance the benefits of each, though decisions should always be made with a clinician who can tailor treatment to individual risks and goals.
“You’ve talked a lot about the benefits of these drugs, but what about the side effects?” asked Evan from North Carolina. “These are new drugs. Isn’t there a lot we don’t know about their long-term effects?”
Evan asks an important question. While GLP-1s have exploded in popularity in the past few years, they’re not entirely new. The first medication in this class, exenatide, was approved in 2005 to treat diabetes. That means we already have about two decades of safety data from millions of people. The most common side effects are gastrointestinal (nausea, vomiting, diarrhea and stomach cramps), which tend to lessen as the body adjusts. More serious issues, such as pancreatitis and gallbladder disease, have been reported but remain uncommon.
That said, it’s always possible that long-term or rare effects could emerge as use broadens to new populations. For example, GLP-1s are now approved for people with heart failure and chronic kidney disease, groups that tend to be more medically frail and may experience different or more severe side effects. Scientists and regulators must carefully monitor these potential consequences and advise patients accordingly.
As with any treatment, the question isn’t just whether a drug has risks, but whether its benefits outweigh the risks of not treating the condition. In the case of obesity, that includes a higher likelihood of heart attack, stroke, multiple cancers and shorter lifespan.
The post Can GLP-1s address infertility? Answering your questions about the drugs. appeared first on Washington Post.